New Prostate Cancer Breakthrough Raises Hope; But There’s a Catch Doctors Aren’t Talking About Yet
Prostate cancer remains one of the most challenging health issues for men worldwide. But in recent months, researchers have made remarkable strides, unveiling what many are calling a prostate cancer breakthrough; a combination of fresh imaging techniques, new targeted therapies, and re-energized immunotherapy efforts. For patients and their loved ones, it can feel like the tide is finally turning. Yet, as with many breakthroughs, there’s a catch: not everyone will benefit equally. And some of the limitations are not being widely discussed.
In this post, we’ll walk you through what’s new, what’s promising, and what you should know before placing all your hopes on the latest headlines.
What’s Driving the Latest Prostate Cancer Breakthrough
• Better imaging: Finding cancer more precisely
One of the biggest advances underlying recent progress is the improved ability to detect and map prostate tumors, even when they’re small or hidden. A 2025 study described a new AI-enhanced imaging system that combines MRI and ultrasound (TRUS), outperforming radiologists in identifying clinically significant prostate cancer (CsPCa). The multimodal AI detected more lesions with higher specificity and fewer false positives compared to standard approaches. (arXiv)
Moreover, new imaging methods like a time-dependent diffusion MRI (TDD-MRI) combined with machine learning promise to further refine detection while potentially reducing unnecessary biopsies. (arXiv)
Having more accurate imaging means doctors can better tailor treatments: for some men, that could mean less invasive care, or even avoid surgery altogether.
• Targeted therapy: Hitting cancer; not healthy tissue
Perhaps the most visible “breakthrough” in headlines is the rise of targeted radioligand therapy. The drug Pluvicto (lutetium-177 vipivotide tetraxetan) has emerged as a game-changer. Pluvicto binds to a protein called PSMA (prostate-specific membrane antigen), which is abundant on many prostate cancer cells, then delivers radiation directly into those cells, sparing healthy tissue. (Stanford Medicine)
Pluvicto was already FDA-approved for advanced, treatment-resistant prostate cancer (metastatic castration-resistant cases), but in 2025 its use expanded in many clinics to offer it earlier in the treatment process, sometimes even before traditional chemotherapy. (Stanford Medicine)
Beyond Pluvicto, researchers are exploring next-generation targeted therapies. For instance, an experimental radiopharmaceutical called 225Ac‑PSMA‑R2 combines a potent alpha emitter with PSMA targeting, aiming to deliver even more destructive radiation to cancer cells while limiting side effects. The therapy is still in early (Phase I/II) trials as of mid-2025. (Wikipedia)
Who Benefits Most from the Latest Prostate Cancer Breakthrough?
The prostate cancer breakthrough is especially life-changing for men who:
-
Have PSMA-positive tumors
-
Have metastatic castration-resistant prostate cancer
-
Have failed chemotherapy
-
Have limited remaining treatment options
-
Live near advanced oncology centers
Early responders see:
-
Reduced tumor burden
-
Delayed progression
-
Lower PSA levels
-
Improved quality of life
This makes the prostate cancer breakthrough one of the most hopeful developments in decades.
Who May NOT Benefit From the Prostate Cancer Breakthrough?
Men may not benefit if:
-
Their tumor lacks PSMA
-
They have neuroendocrine prostate cancer
-
They lack access
-
They have kidney issues or bone marrow suppression
-
They cannot tolerate radiopharmaceuticals
These exclusions are why we must talk about the catch behind the prostate cancer breakthrough.
Navigating the Prostate Cancer Breakthrough: Essential Questions to Ask Your Doctor
-
“Is my cancer PSMA-positive?”
-
“Do I qualify for the prostate cancer breakthrough treatment?”
-
“What are the risks of this prostate cancer breakthrough for someone my age?”
-
“What alternative breakthrough options are available?”
-
“Are there clinical trials involving this prostate cancer breakthrough?”
These questions empower you to get clarity.
The Future of the Prostate Cancer Breakthrough Movement
Researchers predict more prostate cancer breakthroughs in:
-
Alpha-particle radiotherapy
-
Personalized immunotherapy
-
Gene-editing strategies
-
Deep-learning imaging
-
Multi-modal precision therapy
It’s clear:
We are entering a golden age of prostate cancer breakthroughs.
But we must stay cautious, informed, and realistic.
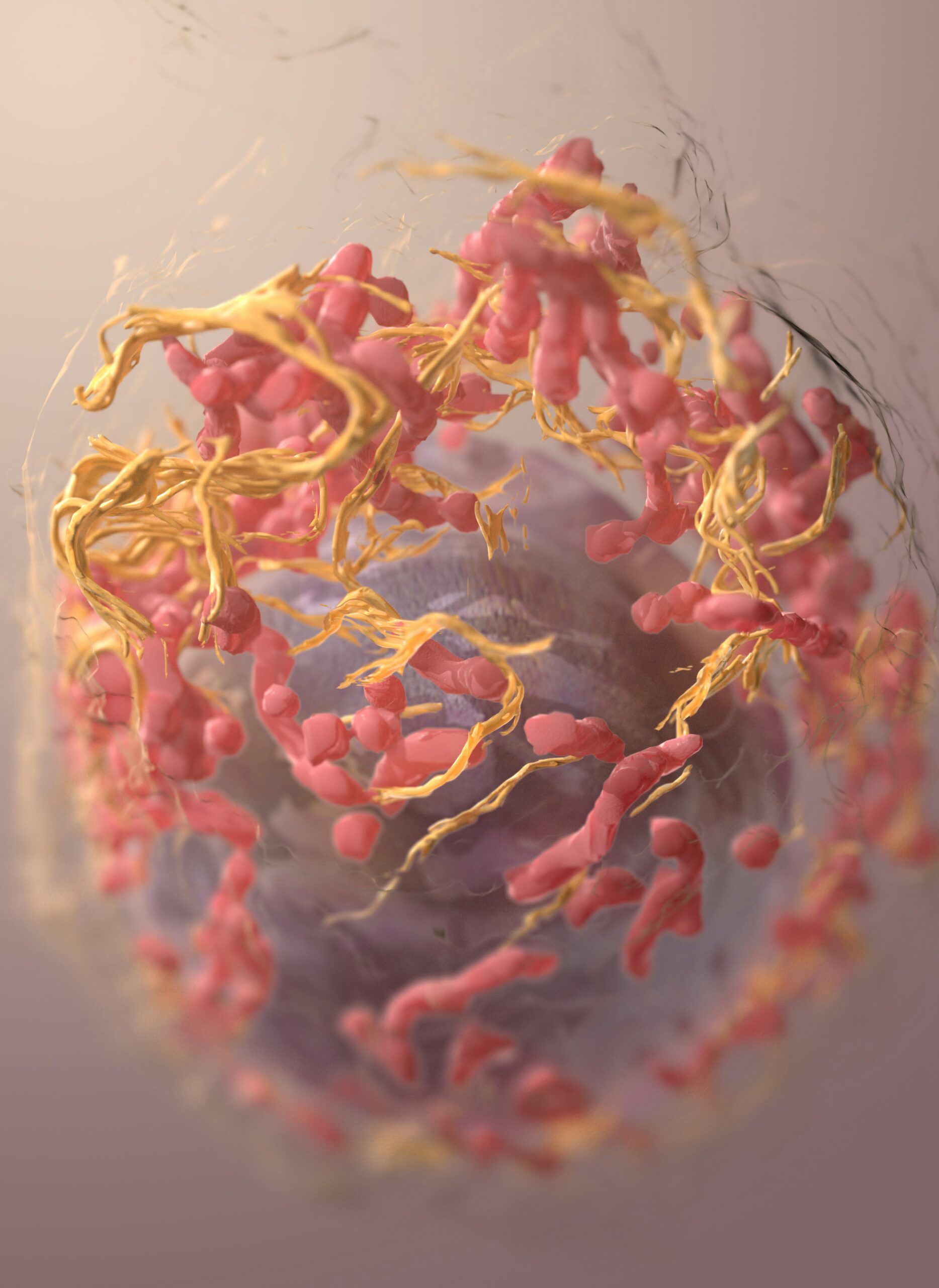
• Immune system + smart medicine: Awakening the body’s defenses
For years, prostate cancer had seemed resistant to immunotherapy. But that may be changing. Researchers at University of Arizona Health Sciences recently demonstrated that by first inhibiting a protein called PIM1, present in tumor-associated macrophages, then applying immune checkpoint inhibitors, tumors that once ignored immune attack became vulnerable again. (ScienceDaily)
Separately, a small clinical trial at Icahn School of Medicine at Mount Sinai used a “viral-mimicking” drug injected directly into prostate tumors before surgery. The goal: wake up the immune response locally and help the body recognize and destroy cancer cells. Early results were safe and even showed early signs of immune infiltration in the tumors. (Mount Sinai Health System)
In addition, novel approaches from nanomedicine are being developed, for example, a therapy using lipid nanoparticles to deliver mRNA and siRNA to cancer cells, which aims to restore tumor-suppressor functions while silencing tumor-promoting ones. Early lab results are encouraging. (BIOENGINEER.ORG)
Why This Breakthrough Matters; Especially for Advanced or Hard-to-Treat Cases
- Improved quality of life: Traditional prostate cancer treatments, surgery, broad radiation, aggressive chemotherapy, often come with side effects: incontinence, sexual dysfunction, damage to nearby tissues. Targeted therapies like Pluvicto minimize collateral damage by zeroing in on cancer cells.
- Options when hormone therapy fails: Many men with advanced prostate cancer eventually develop resistance to standard hormone-blocking therapies. Radioligand therapies or immunotherapy offer new lines of defense when older options no longer work.
- Reduced need for invasive procedures: With better imaging and smarter diagnostics, some men could avoid biopsy, surgery, or aggressive radiation, or at least delay them.
- Personalised approach: By combining imaging, molecular profiling, and immune/treatment response predictors, doctors can tailor therapies for each patient.
Let’s look at a quick comparison of some of the major recent advances:
| Therapy / Innovation | What It Does | Key Benefit | Current Status (as of 2025) |
|---|---|---|---|
| PSMA-targeted Radioligand Therapy (e.g. Pluvicto) | Delivers radiation directly to PSMA-positive cancer cells | Minimizes harm to healthy tissue; effective even in metastatic, hormone-resistant prostate cancer | FDA-approved; expanding use earlier in treatment cycle (Stanford Medicine) |
| Alpha-emitter Radiopharmaceutical (225Ac-PSMA-R2) | High-energy alpha radiation to destroy cancer cells | Potential for stronger tumour-killing with minimal healthy tissue damage | Phase I/II clinical trials ongoing (Wikipedia) |
| AI-enhanced Imaging (MRI + Ultrasound + AI, TDD-MRI + ML) | Improves detection, reduces false positives/negatives | More accurate diagnostics → less over-treatment, better tailored care | Early studies; promising results (arXiv) |
| Immunotherapy + Macrophage reprogramming (PIM1 inhibition + checkpoint inhibitors) | Reawakens immune response against prostate tumors | Offers possibility of long-term control without radiation or surgery | Lab and animal-model success; human trials expected (ScienceDaily) |
| Neoadjuvant Immune-activating Injection before Surgery | “Primes” tumour so immune system recognises and fights it | Boosts effectiveness of traditional surgery; may reduce recurrence risk | Phase I trial with encouraging early results (Mount Sinai Health System) |
| Nanoparticle-based mRNA/siRNA therapy | Restores tumour-suppressor genes, silences cancer-promoting genes | Fine-tuned molecular therapy; potentially fewer side effects | Preclinical / early-stage research (BIOENGINEER.ORG) |
The Catch Doctors Aren’t Talking About; Why It May Not Be a Universal Fix Yet
Despite the excitement, it’s important to recognise that these breakthroughs come with limitations. Here are some of the warnings and caveats you probably haven’t heard loudly discussed:
⚠ Not every prostate cancer patient will benefit
- PSMA-positive requirement: Targeted therapies like Pluvicto or PSMA-based radiopharmaceuticals only work if the cancer cells express PSMA. Not all prostate cancers do. That means some men, even with advanced disease, may not be candidates.
- Tumor biology matters: Aggressive or atypical prostate cancers may not respond, even if PSMA-positive; some subtypes may evade these therapies.
- Immune therapies are still uncertain: Promising immunotherapy strategies remain largely in early research or clinical trial phases. It may be years before they are widely available, if they succeed.
⚠ Access, Cost, and Infrastructure
- Advanced imaging and radioligand therapy require specialized equipment and trained professionals. In many low-resource settings, including parts of Africa, availability may be limited.
- High cost: Radiopharmaceuticals, especially newer ones, can be expensive; and insurance/healthcare coverage may lag behind.
- Limited long-term data: Because many of these therapies and approaches are recent, we don’t yet have robust long-term outcome data (e.g., survival at 5, 10, 15 years, quality-of-life over time).
⚠ Overhyping vs. Reality: What headlines may gloss over
Media stories often frame breakthroughs as “cures” or “game-changers,” but the reality is more nuanced. These therapies may extend life or delay progression, but not necessarily eliminate cancer entirely. For many men, prostate cancer remains a chronic condition, albeit more manageable.
Moreover, early success in labs or small trials doesn’t guarantee broad effectiveness. Some technologies may fail later in large-scale studies.
What This Means for Patients and Their Families: Questions You Should Ask
If you or a loved one is facing prostate cancer, here are important questions to discuss with your doctor; to get clarity on whether the “breakthrough” applies to you:
- Is the cancer PSMA-positive? Ask about PSMA imaging or PET scans — that determines eligibility for PSMA-targeted radioligand therapy.
- What subtype of prostate cancer do I have? Genetic/molecular testing can reveal whether the tumor will likely respond.
- What are the risks vs. benefits of newer therapies vs. traditional treatments (surgery, radiation, hormone therapy)?
- What is the cost and availability of advanced treatment at my hospital/region?
- Are there clinical trials I can join? Sometimes, access to the newest therapies is only via trial enrollment.
- What data is available about long-term outcomes? Since many breakthroughs are recent, ask what is known, and what remains uncertain.
Looking Ahead: How We Can Make the “Breakthrough” More Equitable and Effective
The recent advances represent huge promise; but realizing that promise for all men with prostate cancer will require more than just new drugs. Here’s what needs to happen:
- Wider access to diagnostic imaging and PSMA testing, especially in regions with limited resources. Without detection, targeted therapies can’t be offered.
- Expanded clinical trials globally, not just in wealthy countries; to test how effective and safe these therapies are across diverse populations.
- Long-term follow-up and data collection, to assess not just immediate benefits, but survival, quality-of-life, side effects, and relapse rates over time.
- Public awareness without hype; balanced information so patients understand both potential and limits.
- Integration of conventional treatments with new therapies, creating personalized, hybrid treatment plans rather than replacing established approaches wholesale.
Final Thoughts; Hope, With Eyes Wide Open
The current wave of innovation in prostate cancer, improved imaging, PSMA-targeted therapy, revived immunotherapy, nanomedicine, is nothing short of remarkable. For many men, it could mean more years, better quality of life, and less fear of invasive surgery or debilitating side effects.
But it’s not a silver bullet. The “breakthrough” is real, yet it remains a work in progress. Biology, access, cost, and long-term data all pose serious challenges. And that’s why it matters that patients, families, and doctors engage in open, honest conversations about risks, benefits, eligibility, and realistic expectations.
If you or someone you know is dealing with prostate cancer, use these advances as a source of hope, but treat them as tools to talk over with your care team, not magic wands.
Because with breakthroughs comes responsibility: to understand them, respect their limits, and push to make the benefits real, for as many people as possible.